What is Blood-thinning Medication?

Blood-thinning medication is designed to dilute the blood and make it less prone to clotting. It is a common necessity for many patients with cardiovascular diseases. But is there a need for dietary restrictions when taking blood thinners? Are there significant side effects? Read on to discover more.
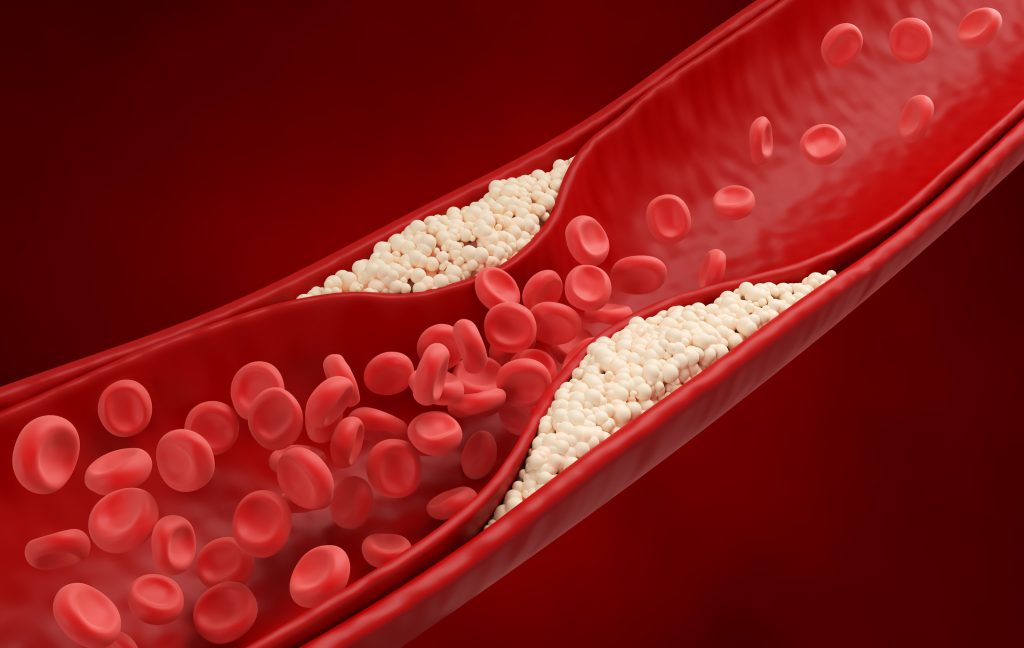
Blood Clothing Process
When a blood vessel ruptures and bleeds, the blood takes two steps to stop the bleeding. First, platelets are adhesive molecules, and when a blood vessel is damaged, they attach to the injury site to form a clot and seal the wound. This is initially very unstable, so a network of brin, made up of proteins called “clotting factors,” strengthens it. Clotting factors and platelets stick together at the wound’s surface to form a clot, thus stopping the bleeding.
What are Blood Thinners?
Blood thinners are medications that dilute the blood and make it less likely to clot, divided into two types: anticoagulants and antiplatelet drugs. They effectively prevent blood clots from forming or stop existing clots from growing, ensuring smooth blood flow.
Anticoagulants
In the clotting process, anticoagulants interfere with various clotting factors, slowing down the related processes. Oral anticoagulants can be categorized into:
Typical oral anticoagulant:
Vitamin K antagonists (e.g., warfarin), Direct thrombin inhibitors, Direct factor Xa inhibitors, etc.
Antiplatelet Drugs
Antiplatelet drugs reduce platelet aggregation and inhibit clot formation. The process of platelet activation involves several activators like thrombin, thromboxane A2, and adenosine diphosphate, amplifying the platelet response and stimulating aggregation.
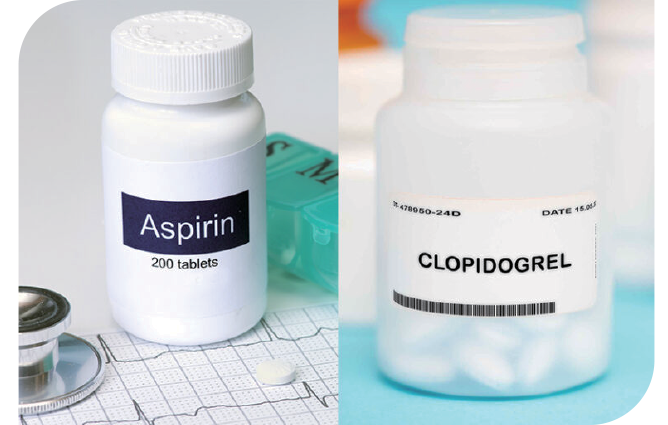
Typical oral antiplatelet drugs:
Cyclooxygenase-1 inhibitors (e.g., aspirin), Thienopyridine, Adenosine triphosphate analogues, Phosphodiesterase inhibitors, etc.
Are There Dietary Restrictions When Taking Blood Thinners?

The Most Common Side Effect is Bleeding
These medications may make you more prone to bleeding in various body parts, such as nosebleeds, gum bleeding, blood in urine, or heavier menstrual bleeding. If you experience these symptoms, do not stop taking the medication or reduce the dosage on your own, immediately consult a doctor or pharmacist. Depending on the nature of surgery or treatment and the medication you are taking, you may need to stop taking these medications, so it is crucial to inform your doctor if you are on blood thinners before undergoing surgery or treatment.

Be Cautious With Certain Foods
When taking Warfarin, dietary restrictions are necessary. Avoid spinach, watercress, liver, black fungus, green tea, natto, avocados, etc., as they are rich in vitamin K, which helps the liver produce blood clotting molecules, enhancing the clotting function. Excessive vitamin K intake can reduce the effectiveness of Warfarin, making it easier to form clots. Seaweed, such as kelp and sea lettuce, also contains vitamin K and should be consumed in moderation. The new generation of blood thinners – Direct Thrombin Inhibitors, does not require special dietary restrictions, but patients can consult their doctors for more details.

When Having Check-ups, Surgeries, or Dental Treatment
The timing for stopping the medication depends on the type of drug, surgery/ treatment, and the patient’s condition. Therefore, inform your doctor about the medications you are taking and follow the doctor’s instructions. Do not stop the medication on your own.

Q: Can you enjoy the benefits of fucoidan while on blood thinners?
Absolutely! Fucoidan does not impact the platelets
responsible for blood clotting, so it does not affect either platelet loss or the clotting function. What’s more, combining fucoidan with anticoagulants and antiplatelet medications like Warfarin and Aspirin is safe. If you have any concerns, consider reducing the amount of fucoidan, and consult your primary care physician for personalized advice.
